The skin is the largest organ in the human body. Its barrier function keeps us hydrated and protects us against the innumerable harmful attacks from pathogens and substances from the environment. But once in a while, the protective function of the skin may be affected by either an internal or external factor. That is when the skin needs our attention, and perhaps the trained eyes of a doctor too.
Below we will go through the most common skin issues our doctors receive at the clinic in Singapore. The article is not meant to be a self-diagnostic tool. Rather, it aims to provide an overview of what broad problems your skin might be experiencing, how to take essential self-care, when to see a doctor, and how not to exacerbate it at home.
Table of Contents
1. The ‘Issues’ with Skin Issues in Singapore
If you are under the impression that skin problems are prevalent in Singapore, you are probably right. Skin issues are among the chief complaints doctors receive here. A number of factors might contribute to this trend.
Firstly, the constantly hot and humid weather tends to make us perspire more, which can stress out the skin and strain its barrier function. With excessive sweating comes heat rash, skin irritation and even bacterial infections. In fact, a study has established the linkage between rising temperatures and the prevalence of skin concerns, in particular eczema and dermatitis (i.e., inflammation of the skin). High humidity at home is a favourable environment for house dust mites - another trigger for some individuals with chronic eczema.
The incidence of skin issues is found to increase with age. Ageing causes the skin to lose its elasticity and thickness. For some seniors, the accumulated impact of sun and other environmental exposure over the years can also weaken the skin. For others, medications they take to manage an unrelated condition may increase the skin’s sensitivity. On the surface, we see elderly people with more wrinkles, age spots, and drier skin. What we cannot see but may experience as we grow older is that the ageing skin tends to be prone to disorders and injuries. For instance, shingles - a viral infection affecting the skin - is common among people over 50 years old. With the ageing population in Singapore, it is natural that skin complaints are becoming more prevalent.
Our personal habits can add further stress to the skin. The habit of frequent handwashing with soap is crucial to fight Covid-19, but it can cause our hands to dry out, flake and even bleed. Similarly, unsuitable skincare and cosmetics or exposure to harsh cleaning products can irritate the skin, causing allergic reactions or other skin problems. Adding it all up, our skin needs to be cared for in more ways than just using skincare and lotion.
2. Common Skin Issues in Singapore
Below are some of the common skin problems you need to be aware of, together with a brief description for each of them. Click the individual conditions below to find out more:
- Skin rashes: a typical skin symptom with various causes, ranging from heat rash, hives, skin allergy, to eczema, shingles, and more.
- Eczema: A group of non-contagious inflammatory skin conditions affecting adults as well as babies. It typically causes the skin to be dry, red and itchy.
- Psoriasis: A chronic non-contagious inflammatory skin disease characterised by red patches and white scales.
- Skin infection: The skin can become infected by bacterial, fungal or viral sources. Examples include ringworm, athlete’s toes, nail infection, shingles, herpes, and certain types of acne.
- Skin ulcer: Mouth sores, shoe blisters are minor skin ulcers we might experience from time to time. More serious types of skin ulcer happen due to the lack of blood flow to the skin, as in the cases of pressure ulcer (i.e., pressure sore) or vascular ulcer (stasis ulcer).
- Abnormal skin growth: A new skin tag or skin spot can be frequent sights as we age. In rare cases they can be cancerous. Detected early, skin cancer is highly treatable. Be sure you have all abnormal skin growths checked by a dermatologist as soon as you identify them.
3. Skin Rashes
A skin rash is often the earliest sign we notice when we have a skin disorder. It may look like a pink or red itchy patch that does not go away, or a swollen lump that seems to appear out of nowhere. You may hear doctors refer to it as a dermatitis rash.
A rash is a symptom and not a skin condition by itself. It can be triggered by heat and trapped sweat (i.e., a heat rash), a bug bite, an allergic reaction, or an underlying skin condition such as eczema, psoriasis, or shingles. Due to the multiple presentations and causes of skin rash, you may need to visit a doctor or dermatologist to be properly diagnosed.
Should I self-treat my rash with over-the-counter cream?
Most rashes are temporary and will get better on its own in a few days. You can relieve itchiness with over-the-counter anti-itch cream. It is also advisable to keep the area clean, dry and open to the air to promote healing.
When do I need to see a doctor for a rash?
In general, a rash that lasts more than a week or shows up with other symptoms should be checked by a healthcare professional. If your rash is accompanied by a fever, it could indicate an infection, or a disease like shingles or measles. See a doctor if the rash does not improve in a week with home care, is spreading, looks and feels worse, becomes infected, or if you develop other symptoms.
Seek urgent medical care if you have rashes together with trouble breathing, swollen lips or tongue, vomiting, or if the rash spreads very quickly. You may be having a severe allergic reaction.
Should I see a GP doctor or dermatologist for a rash?
General practitioners, family doctors and dermatologists can all treat skin rashes. Visit your regular doctor or find one that is most accessible to you. However, if you suspect your rash is caused by a severe allergic reaction, head down to the nearest A&E immediately.
How to care for a rash at home?
To promote healing from a rash, make sure you practise the followings:
- Use only mild cleansers to clean it. You can also clean the rash with just water.
- Always keep the area clean, dry and open to air.
- Apply anti-itch cream or use cold compress to soothe the rash if it is itchy or uncomfortable.
- Treat it gently and take more rest - sometimes rashes are triggered by stress.
- Refrain from scratching, scrubbing or rubbing on the rash.
- Don’t apply cosmetics or use baby powder on the rash.
- Don’t expose the rash to strong sun, put a bandage or other harsh treatment on it.
- Don’t use hot water or rubbing alcohol to disinfect the rash. You may make it dryer and more irritable.
4. Heat Rash
Heat rash - also called prickly heat or sweat rash - as the names suggest, occurs when heat makes us sweat a lot and some of the sweat is clogged in the skin. Tiny irritable red dots appear in patches, often in areas where sweat collects, such as at the back, chest, armpits, thighs, elbows or back of the knees. In some people, heat rash may look like small swollen lumps or clear blisters. It is more common among adults in hotter months in Singapore. It also affects babies whose sweat glands are still developing. The medical name for heat rash is miliaria.
In many cases, you can safely treat heat rash at home, using the same guide for general skin rashes above. Be sure to monitor if the rash worsens, especially for babies, elderly people, or those with weakened immunity. This is because these individuals are more susceptible to infections and other complications and may need more aggressive treatment to treat the rash.
To prevent heat rash, wear loose breathable clothing. Lightweight cotton is an excellent material for babies and adults alike. If you exercise, choosing a cool environment or timing to avoid overheating, allowing time to cool down and wiping off your sweat regularly during the workout can help.
5. Chafing
Skin chafing is another skin issue caused by sweat combined with friction. Different from heat rash, the main cause of chafing is repeated friction, not trapped sweat. Minor injury on the skin surface starts to occur when it is rubbed continuously against another part of the skin or clothing, and damp skin due to sweat makes it worse.
Chafed skin may look like a pink or red flat patch. It often stings when touched or further rubbed against. More severe chafing can cause blisters, swelling, bleeding and feel very painful. It commonly happens at areas where the skin repeatedly rubs against skin, or clothing, such as the inner thighs, armpits, feet, buttocks, or under the breasts. Chafing is relatively common among marathon runners, bikers and triathlon athletes.
Mild chafing can be managed at home with cleaning and drying the chafed area, applying ointment used for minor cuts and wounds and letting it rest. It is important to avoid the activity that caused chafing until you are completely healed. Seek medical care if the chafing worsens or gets infected.
To prevent chafing, avoid wearing too tight clothes, including inner wear. Petroleum jelly and anti-chafing ointment can provide a protective layer to skin areas that are prone to chafing, such as the inner thighs. For those who exercise, investing time and effort to find well-fitted sports clothes and footwear pays off. Seamless designs and quick dry materials are often your best bet. If possible, stop the activity or change positions when you notice the first sign of chafing. Continuing rubbing on chafed skin will only exacerbate the issue, eventually leading to longer recovery.
6. Hives
Hives are reddened, swollen and itchy areas on the skin caused by an allergic reaction of the body. Hives can be small bumps or large splotches. The ways it looks give it other names like weals and welts. Its medical name is urticaria.
A doctor or dermatologist can diagnose hives quickly by looking at it. What is harder to figure out is what causes the allergic reaction, as there can be various factors, and we do not always know for certain what we are allergic to. People may get an allergy when they eat seafood, nuts, wheat, or spicy food, or take some medications. Bug bites can cause hives too.
Treatment for hives mainly involves treating the underlying allergy. You may require prescribed oral antihistamines or corticosteroids to quickly control allergic symptoms including hives, depending on the severity of your allergy. In mild cases, soothing the hives with an anti-itch cream, cold compresses and other self-care steps may suffice.
For some people, the condition does not come back after treatment. For others with chronic allergy and hives, identifying the allergens (i.e., what causes the allergic reactions) is essential to prevent flare ups. A skin prick test or blood test may be ordered to find out the triggers. At home, keeping a food diary can reveal if you have developed an allergic reaction to some types of food. Knowing your triggers will help you prevent uncomfortable bouts of allergy and hives.
7. Allergic Contact Dermatitis
This is an allergic reaction due to contact with a substance that causes a skin allergy. These substances may include cosmetics ingredients, fragrances, jewellery, latex (such as when using gloves), certain plants or flowers, etc.
Often, the person with an allergy rash can identify what causes the allergy. Avoiding the irritants helps the rash to subside and to prevent it from occurring again. For instance, if you develop a rash on your face after trying a new cosmetics product, the new product may be the cause and you can try discontinuing it to check if the rash gets better.
To relieve discomfort and promote skin recovery, apply the same self-care steps as with other types of rash. Allergy rashes usually improve after one to two weeks without any further contact with the allergens. See a doctor if the rash does not improve with home care and after you avoid all possible allergy causes, or if symptoms worsens quickly - you may be having a severe allergic reaction and in need of urgent medical care.
8. Eczema
Eczema is an umbrella term for a group of inflammatory skin conditions that cause dry itchy skin patches. Atopic dermatitis is the most common type of eczema. Eczema can look similar to a rash, but they are not the same. In people with very dry eczema patches, the rash can resemble psoriasis (discussed in the next section).
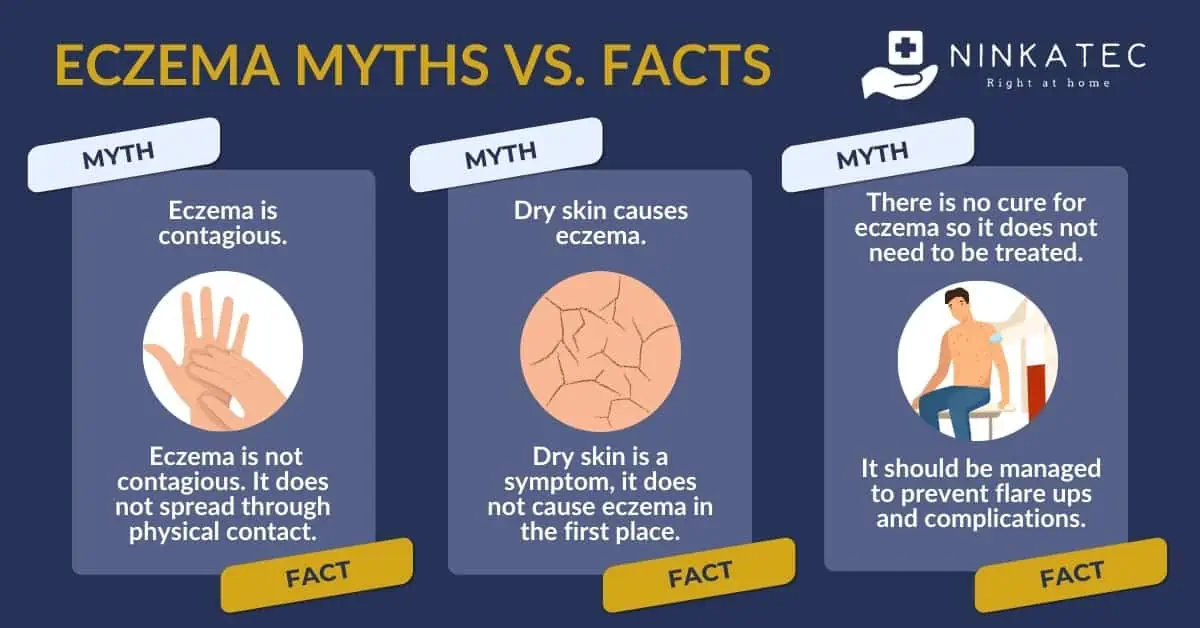
Diagnosing eczema requires investigation of the patient’s history, existing medical conditions, other risk factors and may require a skin biopsy, in addition to physical skin examination. Therefore, it needs to be done by a healthcare professional. In some cases, you may be diagnosed with a rash first, and later on with eczema, after the doctor has gathered sufficient clinical evidence to make such a diagnosis. It is not known what exactly causes eczema, but most researchers agree that it is a combination of environmental triggers and the body’s immune reaction. Eczema is not contagious.
Eczema is a chronic skin condition, which means that it can be managed, but cannot be cured. Eczema management aims to prevent flare ups and complications. To do that, you need to follow the doctor’s treatment plan, take self-care measures to accelerate recovery, and avoid scratching, irritations and infections to the affected areas when you experience symptoms.
The best way to prevent flare-ups is to know your triggers and avoid them. There are a number of common irritants, but eczema triggers for one individual may differ from another. It is important to know and manage yours.
Generally, eczema is known to be triggered by:
- Home and workplace irritants such as house dust mites, moulds, dust, pollen, pet dander, the smell of new paint, or other strong artificial smells
- Hot and humid weather (an ideal environment for dust mite and mould)
- Cold, dry weather (e.g., when you travel to cold countries in winter)
- Soap, bath products, detergents, cosmetics, fragrances, etc that irritate the skin
- Excessive perspiration, skin rashes, skin infections
- Stress, hormonal changes
Note that people with eczema can be more susceptible to skin infections. Vaccinations such as the shingles vaccine can help you manage the risk of vaccine-preventable infections.
9. Psoriasis
This skin condition is characterised by red skin patches with white or grey scales which may be itchy. Psoriasis rashes can appear anywhere on the body, including the scalp, hands, knees, and face. However, different from eczema, psoriasis is believed to be an autoimmune disease, in which the skin cells grow and shed too fast, creating the distinctive scales.
Some people mistakenly think that psoriasis is contagious because of the way it looks. In fact, it is not contagious and you cannot catch it by coming in contact with someone’s affected skin.
You need the trained eyes of a doctor or dermatologist to tell the difference between eczema and psoriasis and confirm the diagnosis. Treatment for psoriasis includes topical cream to moisturise the skin, reduce scaling and soothe the itchiness. In severe cases, you will need medications to control the autoimmune reactions, which may systematically attack not only the skin but other parts of the body, especially the joints, nails, eyes and lungs.
Since psoriasis is a chronic condition, self-care and managing triggers is critical to prevent attacks. A healthy lifestyle, avoiding skin injuries such as cuts, bites, sunburns, and rashes due to other causes are some of the useful preventive measures.
10. Skin Infections
When germs manage to break through the skin protective barrier, they can cause skin infections. Below are the main types:
- Fungal infection, such as ringworm, athlete's foot, nail infection, yeast infection: Fungi thrive in damp and warm environments. Trapped sweat in non-breathable areas like inside the shoes may put you at risk of fungal skin infection.
- Bacterial infection, such as cellulitis, impetigo, and folliculitis: The risk for this type of skin infection increases in people with eczema, existing rashes or weakened immunity.
- Viral infection, including shingles, herpes, hand foot mouth disease, measles, warts, etc. Shingles and measles can be prevented with vaccines. In Singapore, all adults aged 50 and above are recommended to get the shingles vaccine, as shingles is known to be relatively common among this age group. People without evidence of past infection or immunity should get the MMR (Measles, Mumps, Rubella) vaccine, these viral infections can lead to serious complications.
- Parasitic infection, including scabies, bedbugs: These mites latch on the skin and dig out tiny tunnels to lay eggs, causing the infections.
Symptoms, causes and treatment of skin infections vary from type to type. They may look like a rash, or a fluid-filled blister. Visit a doctor if you are unsure what it is, or if the infection causes you discomfort, has pus, or foul odour. Do not delay your medical visit if you have other accompanying symptoms such as a fever, which may indicate the infection has turned serious. Bacterial infection might need to be treated with antibiotics.
Skin infections are infectious, with the exception of shingles which is caused by the reactivation of the virus that is already dormant in you after a chickenpox episode in the past. You should take care not to share towels, linen, or have prolonged skin-to-skin contact while having a skin infection, especially in the same household.
11. Skin Ulcers
Mouth sores, shoe blisters are minor skin ulcers we might experience from time to time. More severe skin ulcers can be caused by poor blood circulation due to pressure or immobility. Below are two main type of ulcers you need to be aware of:
- Pressure ulcers, also called pressure sores, or bed sores. This type of ulcer commonly develops among people with limited mobility (wheelchair users, bedridden patients), at bony parts of the body that are pressed against over long periods of time (buttocks, shoulder blades, head, heels, etc.) Prolonged pressure cuts off blood flow to the area, damaging skin tissues. Pressure sores can silently develop and thus, tend to worsen quickly if they are not detected early. We wrote a dedicated article about how to care for and prevent them here.
- Non-pressure ulcers: Often affecting the legs, these wounds occur when there is poor blood circulation from the leg, due to damages to the valves of the leg veins or leg nerves. Varicose vein, venous insufficiency and diabetic foot - a complication of diabetes can be the causes. (Learn more about how diabetes causes diabetic foot and other complications here). Treatment of this type of skin ulcers can take a long time and requires management of the underlying cause. Adequate care should be taken to avoid infections at the ulcer sites.
12. Abnormal Skin Growths
Changes to the skin appearance are common as we age. Sun spots (liver spots), skin tags, and new moles may pop up every now and then. The vast majority of them are benign and can be left alone, unless you want to treat them for cosmetic reasons.
In a small number of cases, they can be the signs and symptoms of skin cancer. Although skin cancer is said to be the most visible type of cancer, the untrained eyes might not be able to tell the difference between a mole that indicates cancer and one that does not. Some patients find out they have skin cancer during a visit to the dermatologist to check out what they think of as a completely benign skin issue.
Dermatologists refer to these symptoms as atypical skin spots. Again, not all atypical skin growths are cancerous, but they should always be checked by a skin specialist to be confirmed. Skin cancer is among the top 10 cancers in Singapore, but highly treatable if detected early.
How to identify an atypical skin spot
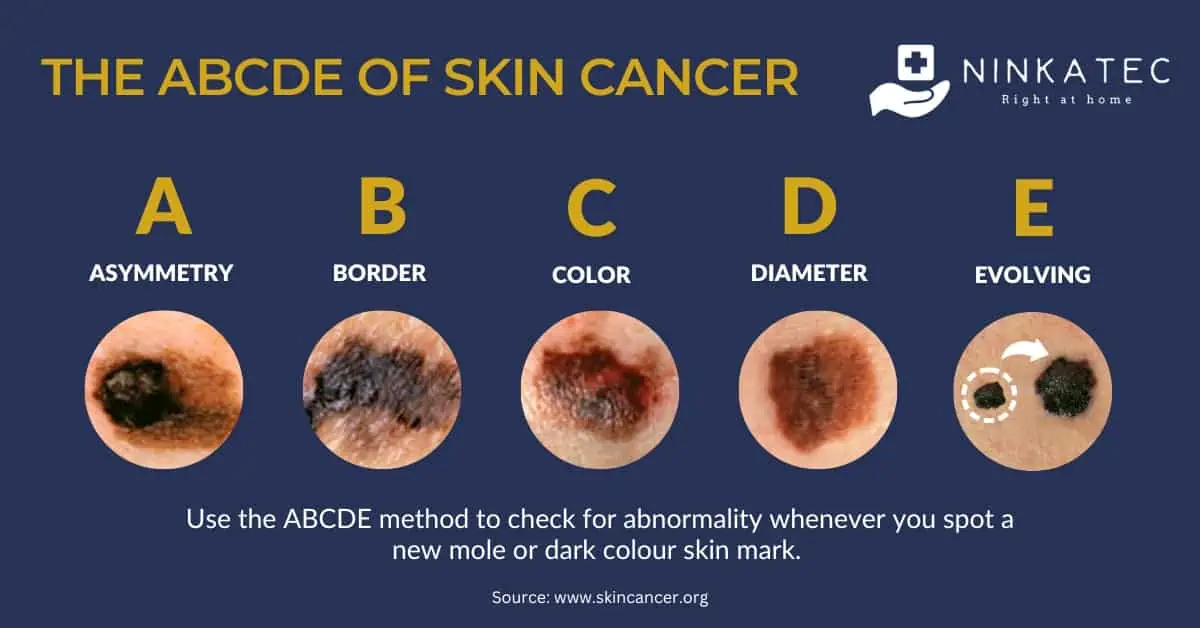
Use the ABCDE method below to check for abnormality whenever you spot a new mole or dark colour skin mark.
[A] Asymmetry – A mole with asymmetrical sides could be the early signs of melanoma - an aggressive type of skin cancer.
[B] Border – Moles with uneven edges, can also indicate melanoma.
[C] Colour – When a mole or skin mark has different shades on it, be sure to have it checked.
[D] Diameter – A mole growing to the size of 6 millimetres or more in a relatively short term should not be left to chance.
[E] Evolving – Seek out the opinion of a skin doctor if you notice the moles, warts or skin marks change in shape, colour, texture, or bleed, or develop crust.
Overexposure to strong sun and age are some of the risk factors of skin cancer. Practising sun safety, wearing sunscreen and covering up when going out in the sun can reduce your risk. If you are a senior or have spent a lot of time in the sun, you may benefit from performing regular skin self-examination or going for skin screening.
13. Takeaway Message
Rashes and skin issues are annoying to deal with, but with awareness and the right care, you can heal and be comfortable in your skin again. Whether you are dealing with a minor heat rash or a chronic skin condition, it is crucial to know your triggers and prevent them. Rashes that do not improve in a week with self-care, rashes that develop with other symptoms, and abnormal skin spots should be examined by a doctor or dermatologist.
Our resident GP doctor at Charazoi Medical Clinic - Dr Choo Dee Pheng - has a special interest in dermatology conditions. Make an appointment or drop in to have her take a look at what is bothering you and your skin during our clinic hours.
Charazoi Medical Clinic – 380 Jalan Besar, #05-01, ARC 380 Singapore 209000, Monday – Friday, 9:00 AM – 12:00 PM | 2:00 PM – 5:00 PM