If you are caring for someone with dementia, you may have found yourself asking “What will happen the day my loved one no longer recognises me?” This heart-wrenching question poses a reality that every loved one expects to face when dementia progresses to the late stage, alongside the many arising day-to-day caregiving challenges.
This article is written to guide you through the complexities of managing severe dementia. We will discuss the progression of dementia, symptoms of severe stages, and considerations to select the best care options for your loved ones. You'll also find practical advice on managing daily care challenges, coping with the emotional toll and ultimately preparing for end-of-life matters when the debilitating disease reaches its final stage.
Table of Contents
7 Stages of Dementia
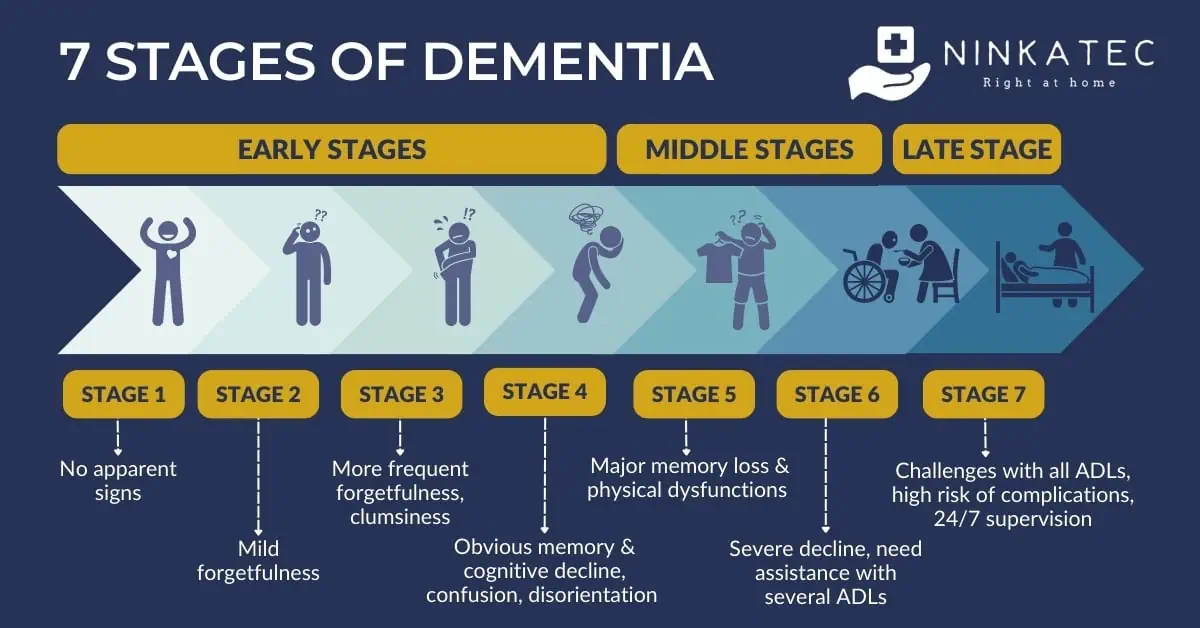
Dementia progresses through 7 levels of intensity, corresponding to 7 stages of cognitive decline. For doctors, it is crucial to accurately identify which stage a dementia patient is in to determine appropriate treatment and care options. For caregivers and family members, understanding the progression of the disease helps you know what to expect and make the most of what is possible at the moment.
For simplicity, the 7 stages are often categorised into early-stage dementia (stage 1-4), mid-stage dementia (stage 5-6) and late-stage dementia (stage 7). Late-stage dementia is also known as advanced dementia or severe dementia.
For the purpose of the article, we will use the terms “late-stage dementia”, “severe dementia” and “advanced dementia” interchangeably to refer to the last two stages of dementia, as transition from stage 6 to stage 7 is not always clear cut. The guides below are useful for both stages of the disease when your loved one experiences, or is expected to experience, a high level of dependency in all activities of daily living.
10 Common Signs and Symptoms of Late-Stage Dementia
The onset of late-stage dementia can occur gradually or suddenly. As a caregiver or family member, you may notice a steady decline in the condition of your loved one over time. Alternatively, specific events, such as hospitalisation or the introduction of a new caregiver, could abruptly worsen symptoms. This sudden change often occurs because people with dementia typically respond best to familiar environments and consistent routines. Any disruption to their usual surroundings or daily patterns can trigger a rapid deterioration.
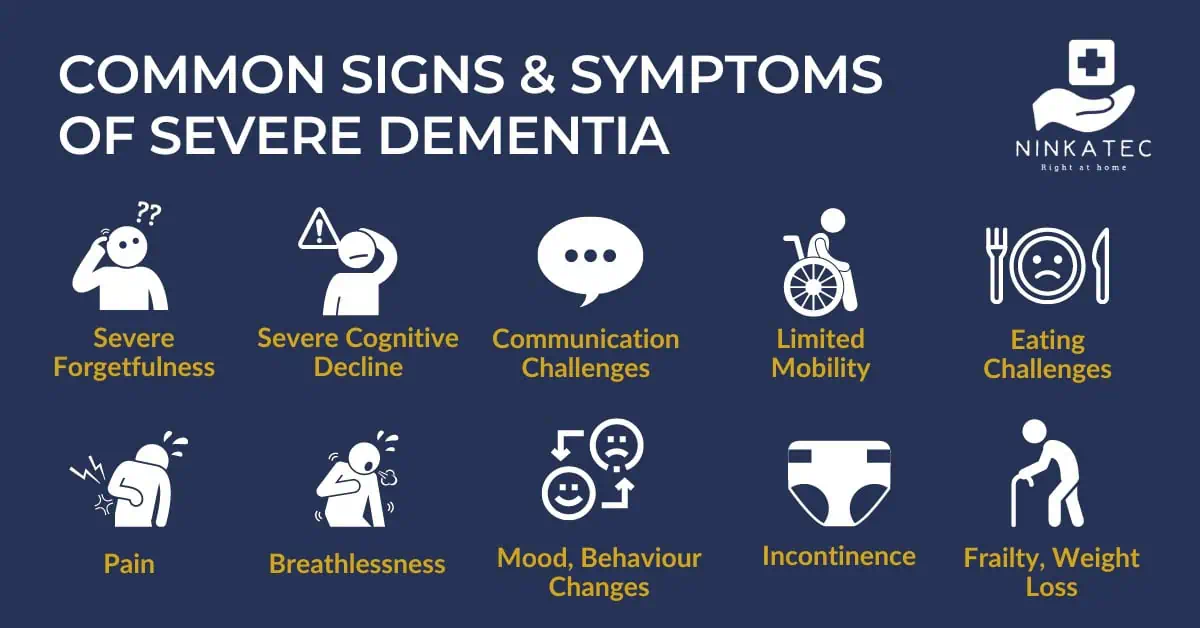
Despite these variations in progression, certain signs and symptoms are commonly observed in late-stage dementia. Understanding these symptoms helps family members and caregivers know what to expect and better manage the challenges that come with this stage.
- Severe memory loss: Dementia in advanced stages can rob a person of the ability to recognise their spouse and children, or themselves when looking in the mirror. They may no longer remember what daily objects such as a toothbrush or a fork is for, making daily tasks more challenging even with assistance.
- Severe cognitive decline: The affected person may struggle to understand conversations or the intentions behind everyday care activities such as bathing or dressing. This can lead to confusion or resistance.
- Severe difficulty with communication: The person may say fewer words which can be hard to understand. Their speech may sound like babbling or nonsensical. Family members may feel like their loved one is gradually losing the ability to speak. This impairment in communication can prevent them from expressing discomfort, and basic needs, such as feeling pain or needing to use the bathroom. As a result, the seniors may react strongly or have emotionally charged outbursts, causing frustration and distress to the caregivers. However, it is important for the family to recognise that babbling and strong reactions are often a form of communication when dementia reaches the last stage.
- Challenges with eating: Late-stage dementia can interfere with appetite and the ability to swallow. The person may eat less, find it challenging to swallow, and keep food in their mouth. Difficulty swallowing may also cause them to cough and choke while eating, increasing the risk of aspiration pneumonia - a serious condition where food particles accidentally enter the lungs.
- Issues with mobility: As dementia advances, your loved one may first show signs of unsteady walking, then gradually losing the ability to walk and stand independently. Over time, they might become chair-bound or bed-bound. Encouraging movement with support can be beneficial, but it is essential to be mindful of the risks of falls and fractures.
- Pain: Pain is a frequent but often overlooked problem in people with dementia, due to difficulties in communication. It is estimated that between 50% and 80% of patients with dementia suffer from pain. Common sources of this pain include muscle and joint pain due to immobility, constipation, and existing conditions such as arthritis or migraine. Additionally, infections, wounds and pressure sores can contribute to their discomfort.
- Breathlessness: In the final stages of dementia, the disease can affect the brain's region controlling essential bodily functions like heart rate and breathing. Shortness of breath can occur, especially among those with existing pulmonary or cardiovascular conditions, such as COPD or heart failure.
- Mood and behaviour changes: Doctors refer to this group of symptoms as behavioural and psychological symptoms of dementia (BPSD). Research shows that up to 97% of dementia patients cared for at home experience some form of BPSD during the course of their illness. Symptoms are typically more prevalent in advanced stages. The person with severe dementia may become more confused and disoriented, restless and aggressive, or upset and withdrawn.
- Weight loss and increasing frailty: Your loved one may lose weight and become increasingly frail, driven by poor appetite, inadequate nutrition, and immobility. The compounding effect of these symptoms can be distressing for families as you witness the physical decline of someone you love.
- Other symptoms: These may include incontinence (lack of control over bowel and bladder functions), increased need for sleep, hallucinations (see, hear or sense things that aren't real, especially at night), delusions (believe things that aren’t real), loss of vision, a mask-like facial expression, etc.
Recognising the symptoms of severe dementia and its implications helps families discuss treatment and care plans with their doctors more effectively. This awareness also prepares caregivers for the evolving care challenges as the disease progresses, allowing you to provide care and support to loved ones with more compassion and less stress.
Treatment and Care Plan for Severe Dementia
In the final stages of dementia, the focus of treatment shifts towards symptom management, ensuring patient comfort, and maintaining quality of life. Whether the person is cared for at home or at a nursing care facility, care primarily addresses basic needs such as nutrition and hygiene, alongside physical support to aid mobility and prevent bedsores.
Medical Treatment for Severe Dementia
To come up with an effective treatment and care plan for late-stage dementia, doctors take into consideration various factors, including:
- Severity and type of dementia
- Presenting symptoms
- Existing comorbidities
- Overall care goals
The recommended plan is the result of both professional assessments and discussions with the patient's family. The objective is to ensure a personalised approach that facilitates round-the-clock care and quality of life for both the patient and family.
It's crucial for families to understand that while there are no drugs to reverse advanced dementia, treatments are available to manage its symptoms. However, the effectiveness of these medications can vary, and they may not always provide the intended benefits.
For instance, antipsychotic medications can be used to treat behavioural and psychological symptoms of dementia (BPSD), but they carry risks, including cardiovascular risks. This makes them unsuitable for patients with heart conditions. Similarly, for patients who have difficulty swallowing, oral medications might increase the risk of complications.
Palliative and Hospice Care
As dementia symptoms become more severe, it may become essential to consider hospice or palliative care options. These approaches involve comprehensive care provided by a team of medical professionals, rather than just a single nurse or doctor. The primary focus of both services is on enhancing comfort and quality of life, which can offer significant relief to both the person with dementia and the caregivers.
However, the difference between hospice and palliative care is that while hospice care is typically provided to patients nearing the end of life, palliative care can be given at an earlier stage of dementia. That said, you don't have to wait until advanced stage of dementia to enlist palliative care. Engaging palliative specialists early in the course of the disease can improve your response to unexpected care challenges. Find out how palliative care can assist you in various aspects of dementia care beyond medical concerns in our article here.
Palliative care service can also facilitate timely preparation for important decisions regarding the healthcare and financial matters of your elderly loved one, such as Advance Care Planning (ACP), Advance Medical Directive (AMD), and Lasting Power of Attorney (LPA). By Singapore law, wills, AMD’s, LPA’s all require the person who makes them is “of sound mind” or certified to be so by a doctor. We highlight the differences of ACP, LPA and AMD here.
How to Manage Complications in Advanced Dementia at Home
For families opting for home care, medical support is often a critical concern. In the advanced stages of dementia, sudden fluctuations in symptoms and complications may increase the likelihood of needing urgent medical care. These complications may include poor oral intake, constipation, falls, infections, and delirium.
To ensure prompt medical care for your loved one with severe dementia, it is advisable to maintain regular contact with a family doctor or GP who can visit the home and recommend the best course of action. For your general knowledge, we go through some of the common complications and strategies for managing them below.
Delirium
Delirium refers to a state of marked increase in confusion or disorientation. It is reported to affect up to one in three people with dementia. Symptoms vary - some patients exhibit obvious signs, while in others, especially those who are withdrawn or sleep a lot, delirium can be difficult to detect.
In patients with more obvious symptoms, you may observe a sudden mood swing or change in behaviour. The senior may suddenly become easily distracted or less aware of their surroundings. Accompanying symptoms might include hallucinations, paranoia, and disrupted sleep patterns. A delirium episode can last a few hours or a few days.
If you suspect your loved one has delirium, contact your doctor for an examination. Unusual increase in the need for sleep should also be reported. The doctor will assess if certain medications or environmental triggers are contributing to delirium, in which case environment adjustments and switching to another medication can help.
In other cases, the cause can be an infection, dehydration or other medical concerns. Treating delirium requires addressing the underlying cause. If delirium persists or worsens, it may require more specialised medical intervention.
In home care, safety is crucial when your loved one is having a delirium episode. They may fall or inadvertently hurt themselves. Make sure the living area is safe and free from fall hazards. Consider safety measures such as bed rails if necessary and do not leave them alone.
Poor Oral Intake
Loss of appetite and difficulties with swallowing can significantly reduce nutrition intake, putting the elderly at risk of malnutrition. While it may be tempting to encourage or "force" your loved one to eat, this can inadvertently increase the risk of aspiration pneumonia - an infection that occurs when food accidently enters the airways. Aspiration pneumonia is one of the leading causes of death among elderly people with advanced dementia.
Faced with this situation, you may consider tube feeding as a logical solution. However, the decision to implement tube feeding requires careful considerations by both the medical professional and the family. Your doctor can help you assess the medical aspect of the decision: Does tube feeding effectively prevent aspiration pneumonia? Can it facilitate the continuation of treatments such as oral antibiotics, thereby avoiding hospitalisations? Can nutrition be supplied by other means?
These medical considerations then need to be balanced with personal preferences and family values. If tasting food is one of the few remaining pleasures and opportunities to bond with loved ones, would it outweigh the medical risk? Without a clear directive and advance planning by the person with dementia, this can be an overwhelmingly difficult decision for the family. Ultimately, the choice should aim to uphold the dignity and quality of life for your senior loved one with dementia and respect their past wishes as much as possible.
Infections
Common infections in dementia patients may include urinary tract infections (UTIs), respiratory infections, and skin infections resulting from pressure sores. Managing infections in seniors with advanced dementia at home requires vigilance and a proactive approach, as infections can quickly escalate and complicate the health of those with compromised immune systems.
In people with severe dementia, infections can manifest as increased confusion, fever, pain, or changes in behaviour. These symptoms should be promptly reported to a healthcare professional for diagnosis. If an infection is diagnosed, your doctor may prescribe oral antibiotics and topical treatments if necessary.
It's also essential to monitor the status of the infection regularly, due to communication challenges your loved one faces at the advanced stages of dementia. Wounds or pressure sores should be inspected daily. Additionally, ensuring hygiene for both the caregiver and the patient is crucial, to avoid the risk of spreading the infection.
Constipation
Constipation is often the result of not drinking enough liquid, which can be common among dementia patients with swallowing difficulty. This condition may also arise from a blockage in the intestines.
To address constipation, doctors typically prescribe laxatives to soften the stool, making it easier to pass. If the constipation is due to a physical obstruction, caregivers might be instructed to perform specific massage techniques to help relieve the blockage.
Your doctor can also recommend ways to improve hydration for people with swallowing difficulty. For example, using alternative liquid forms like gel water or thickened liquids can help prevent future constipation.
Preparing for End-of-Life Care in Late-Stage Dementia
As dementia progresses to its final stage, families often face difficult decisions about their loved ones' care, who are no longer able to make these decisions themselves. These decisions may involve pain management strategies, the use of feeding tubes, or other invasive procedures. An Advance Medical Directive (AMD) or an Advance Care Plan (ACP) can significantly alleviate these pressures.
When these documents are not available and the loved one's wishes are not known, family members will have to make decisions based on what they believe their beloved senior would want.
Here are the essential points to consider when you face these difficult and often deeply emotional decisions:
- Communication with the Care Team: Maintaining consistent and clear communication with the doctor and care team is important to make timely and well-informed decisions.
- Teamwork in the Family: Engaging in open discussions with all family members involved can help the family make more rounded decisions. It can also provide an outlet for members to come together and share feelings and concerns about the impending loss.
- Emotional and Spiritual Care: As our co-founder and CEO - Dr Choo Wei Chieh - reflects after 18 years of providing end-of-life care, physical pain is just one type of suffering at the final chapter of life. Emotional and spiritual needs are no less important. This may involve engaging a social worker or representative from your religion who is familiar with end-of-life matters, or performing meaningful rituals that honour a loved one’s legacy.
- Peer Support for the Caregivers: Connecting with support groups is crucial to relieve stress, find practical advice and help you through difficult times. However challenging and lonely the journey may feel at times, there is someone who has walked your path and can empathise with your feelings if you reach out. In Singapore, you can join support groups run by Dementia Singapore or Caregiving Welfare Association. You can also ask the medical professionals you work with for recommendations.
Legal and Financial Affairs for Late-Stage Dementia
In the final stage of dementia, your elderly loved one often has limited mental capacity, making it too late to obtain a Lasting Power of Attorney (LPA) for family members to act on their behalf.
Without an LPA in place, you can apply to the court to become your loved one's deputy. This process requires a mental capacity assessment conducted by a registered medical practitioner or specialist. Our certified doctors can conduct these capacity assessments conveniently at your loved one's home.
Under Singapore law, deputies must submit annual reports to the Office of the Public Guardian (OPG) explaining decisions and expenses made on the person's behalf. Guidance on obtaining deputyship is available on the OPG website.
Below is a comparison of Deputyship and Lasting Power of Attorney (LPA) for your reference.
Planning and Selecting a Care Option for Late Stage Dementia
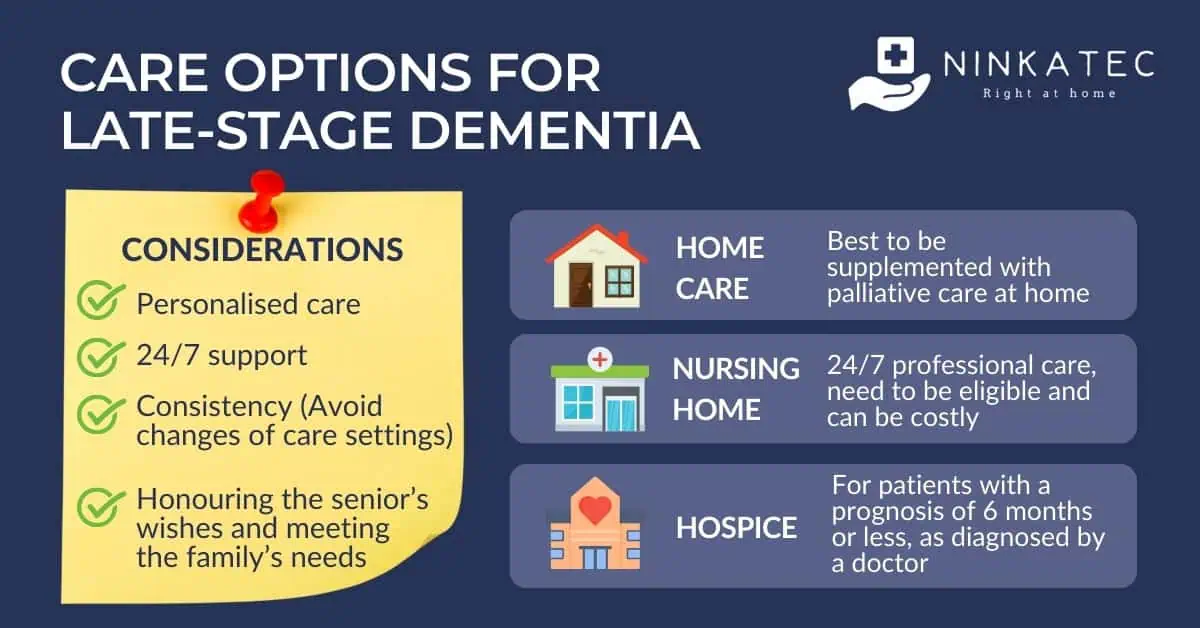
Choosing the optimal care option for a loved one in the late stages of dementia requires understanding the available services and evaluating how well they meet your needs.
Here are some of the available options in Singapore:
- Home Care: This option, when supplemented with home-based palliative care and respite care, allows the seniors to remain in a familiar environment close to loved ones, which is often beneficial for those with dementia. However, home care might not suit everyone. It can be challenging if 24/7 care cannot be adequately provided at home, or if the medical needs are too complex to manage in this setting.
- Hospice Care: Hospice care is designed for patients who are nearing the end of life, typically with a prognosis of six months or less, as diagnosed by a doctor. It is available as inpatient and outpatient services. You can apply for the hospice service you need by getting a referral from the hospital, polyclinic or clinic that your loved one is visiting.
- Nursing Home: Nursing homes provide professional care for dementia patients needing constant medical supervision. This can reduce the caregiving burden on family members. However, in Singapore, there are eligibility criteria to qualify and usually a waitlist for admission.
Each option has its pros and cons. We provide a detailed analysis and comparison of the different options, including costing, to help you weigh your choices in our article here. Ultimately, the best choice depends on your loved one’s medical needs, their personal wishes, and your family resources. When evaluating the choices, bear in mind the following considerations which are specific to late-stage dementia:
- Personalised care: As each person’s experience with advanced dementia is different, care should be tailored to the unique requirement of your loved one.
- Consistency: A stable routine and familiar environment are vital to people with dementia, and frequent changes in care settings should be avoided.
- 24/7 support: Availability of round-the-clock medical support is essential due to potential fluctuations in symptoms.
- Financial and logistical considerations: It’s important to balance costs, accessibility and availability. For instance, available nursing homes that are too far away may not be suitable if you want to see your loved one frequently, or inpatient hospice can be expensive without subsidies.
Takeaway Message
Caring for a loved one with dementia is a path filled with substantial obstacles and deep affection. As a caregiver or a family member, you may feel overwhelmed by daily responsibilities, the complexities of medical decisions, and the distress of watching a loved one decline. However, these very responsibilities underscore your crucial role in your loved one's life. While dementia may rob your loved one of memories and functional abilities, it cannot take away the bond of love and care between you.
At Ninkatec, we understand the paramount challenges dementia patients and caregivers face and the importance of providing support to families that extends beyond traditional care models. By integrating compassionate care with advanced medical technology, we bring reliable 24/7 dementia care to the comfort of your homes. Our care team comprises home care doctors, dementia-specialised nurses, caregivers and other medical services as required.
Medical and care services are provided throughout the dementia care journey of your loved one, including:
- Lasting Power of Attorney (LPA) arrangements while mental capacity remains
- Mental capacity assessment (MCA) for deputyship applications when mental capacity is lost
- Home caregiving tailored to each dementia stage: mild, moderate, and severe dementia
- Palliative and end-of-life care for dementia final stage.
Services can be provided at our clinic in the early stages when your loved ones are able to go out, or in the convenience of your home when commuting becomes a challenge.
Above all, we are committed to ensuring personalised and comprehensive care guided by empathy and compassion for your loved one. Drop us a message below to find out more!