The digestive system is one of the most complex systems in the body, consisting of 10 different organs working together. The body derives energy from nutrients that have been broken down by the digestive system, which is why having good digestion is important for a healthy body. Problems with digestive system however are also one of the most common reasons you have to visit doctors. In part 1 of our comprehensive Gastrointestinal Diseases Guide, we discussed
In the second part of the guide, we cover 5 common stomach and digestive conditions including abdominal pain, indigestion, gastroesophageal reflux disease (GERD), diverticular disease, inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). We also explain about gastroscopy and colonoscopy - 2 procedures commonly used to examine inside our digestive system and diagnose diseases.
Table of Contents
1. Abdominal Pain
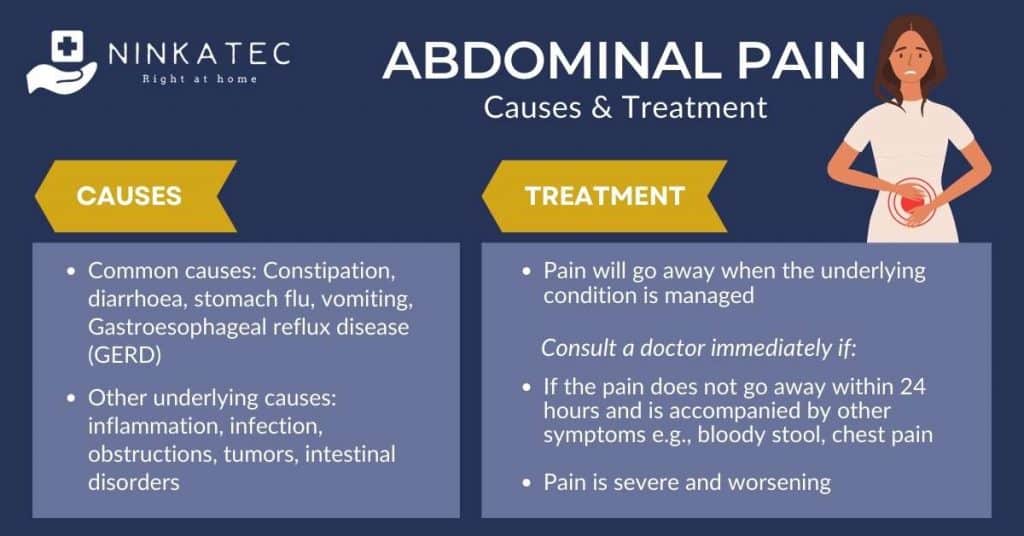
Abdominal pain is a generic term referring to pain felt anywhere in the abdomen, which is between the chest and pelvic. It occurs in various forms and severity levels - crampy, achy, dull, or sharp; acute or chronic. It is a common complaint that affects older individuals, in Singapore as well as all over the world.
Abdominal pain is commonly described by the general public as a stomachache. However, what feels like a pain in the stomach may not be triggered by a problem in the stomach itself. The abdomen houses a large number of organs. Conditions related to any of the organs can trigger abdominal pain. In fact, when you feel abdominal pain, it could signal medical conditions related to:
- Stomach
- Small intestines
- Colon
- Appendix
- Liver
- Spleen
- Gallbladder
- Pancreas
- Kidneys
Doctors would need to assess other accompanying symptoms, order tests and sometimes an endoscopy to determine the underlying cause.
What causes abdominal pain?
The common causes are inflammation, infection, obstructions, tumors, and intestinal disorders.
Infection does not have to be in the stomach area to trigger abdominal pain. When you develop an infection in your throat or blood, the bacteria can also reach your digestive system, causing abdominal pain. When you have a gastrointestinal infection, most often, you will notice bowel movement changes such as diarrhoea or constipation.
In women, besides these causes, cramping associated with menstruation is a prevalent cause of lower abdominal pain.
Common causes of abdominal pain include:
- Constipation - abdominal pain is a common symptom in patients suffering from constipation.
- Diarrhoea - diarrhoea and abdominal pain often occurs together.
- Stomach flu (viral gastroenteritis)
- Gastroesophageal reflux disease (or GERD in short)
- Vomiting
When the pain is severe and requires a visit to the Emergency Room, it could be due to the following conditions which are known to precipitate severe abdominal pain:
- Gallbladder diseases
- Kidney stones or kidney infection
- Pancreatitis (inflammation of the pancreas)
- Appendicitis
- Small bowel obstruction
- Diverticulitis (more on that here)
- Gastroesophageal reflux disease
Types of abdominal pain
When you visit the doctor with abdominal pain, you might hear the doctor describe your abdominal pain as localised, crampy, colicky or generalised. Here are some explanations to what they mean:
- Localised pain comes from a particular area of your abdomen. It usually reflects issues with the organ that sits underneath it. Localising the pain is very helpful for the doctor to determine what is causing it. For instance, if you have upper abdominal pain (under your chest), it may indicate an issue with your stomach or pancreas.
- Crampy pain feels like an involuntary muscle contraction inside your abdomen. It is often sudden and may accompany other digestive symptoms, such as diarrhoea, floating, and gas. In women, pain may be associated with reproductive disorders, for example premenstrual syndrome, miscarriage, tubal pregnancy, ruptured ovarian cyst, or urinary tract infection (UTI).
- Colicky pain indicates bouts of pain that come and go suddenly. This type of abdominal pain is often severe and may mean there are issues such as kidney stones and gallstones.
- Generalised pain is used to describe cases where the pain area is large or when patients cannot identify exactly where the pain is.
Treatment for abdominal pain
Treatment for abdominal pain depends on the underlying condition causing the pain. For common causes such as diarrhoea due to certain types of known food or previously diagnosed constipation, diarrhoea or GERD, pain will typically go away when the condition is managed. However, if abdominal pain persists for more than 24 hours despite self-management, or increases in severity, or presents with other symptoms such as bloody stool, fever, pain in other parts of the body like chest pain or headache, please consult your doctor immediately for further diagnosis and actions.
2. Indigestion (Dyspepsia)
Dyspepsia is the formal term for indigestion, which refers to feelings of discomfort or pain in the upper abdomen after eating a meal. This is not a disease; it is a mere symptom. According to one report, dyspepsia affects 30% of the population, presenting with other symptoms, such as bloating, nausea, and gas.
The treatment of dyspepsia mainly focuses on lifestyle changes, especially when it gets triggered by eating and drinking. Besides food indigestion, dyspepsia can result from GERD and the use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs).
Symptoms of dyspepsia (indigestion)
Almost everyone has experienced bloating and the feeling of indigestion after a heavy meal. There is no need to see a doctor if it is not regular and goes away quickly. However, consult a doctor if dyspepsia happens regularly or persists, or if dyspepsia accompanies other symptoms such as loss of appetite, loss of weight, fatigue, vomiting, blood in stool or vomits, etc.
To diagnose dyspepsia, your doctor needs to document one or more of the following symptoms:
- Abdominal pain (usually the upper portion)
- A burning sensation in the digestive tract
- Feeling bloated after eating
- Other associated symptoms such as nausea, excessive burping
Treatment for dyspepsia (indigestion)
The treatment of dyspepsia is dependent on the underlying cause. As a general rule of thumb, addressing the underlying condition and modifying the patient’s lifestyle lowers the episodes of dyspepsia.
Lifestyle changes
If your dyspepsia is mild with infrequent episodes, your doctor may suggest:
- Avoiding or limiting the intake of trigger foods (e.g., fried foods, chocolate, onion, garlic)
- Switching from soda to water
- Eating smaller meals (5–7 times a day)
- Chewing your food slowly to allow for proper digestion
- Limiting the intake of caffeine and alcohol
- Monitoring your weight to avoid obesity
- Eating your last meal at least 3 hours before bed
- Raising the head of the bed
- Limiting smoking
- Avoiding tight clothes
Medications
If you have severe symptoms that do not respond to the measures listed above, your doctor may suggest a few medications to control the symptoms. Depending on the cause of your dyspepsia, the treatment options will vary greatly. Speak with your doctor about the prescribed medications and their potential side effects on your body.
3. Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease, or GERD, is an extremely prevalent condition in the general population. It is the result of acid regurgitating to your esophagus (i.e., food pipe), which manifests with a burning sensation and abdominal pain. While most people experience acid reflux from time to time, those who display symptoms at least twice a week may have GERD.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), GERD affects around 20% of Americans. The statistic is identical for Singapore, with 1 in 5 Singaporean dealing with GERD. Unfortunately, not treating GERD can lead to severe complications.
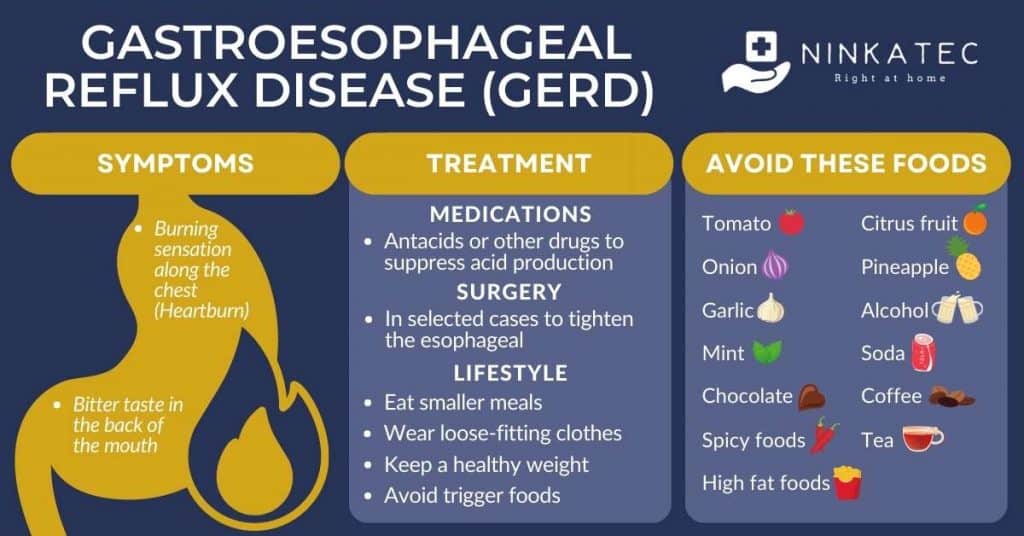
GERD symptoms
GERD presents with several symptoms, including an uncomfortable burning along your chest; people often refer to this symptom as heartburn. Some individuals who have GERD report a bitter taste in the back of their mouths, which is due to acid and food regurgitation.
When the acid leaks to the lungs, it can cause asthma and a serious condition known as aspiration pneumonia.
GERD causes
Scientists identified a defect in the lower esophageal sphincter (LES) as the primary trigger of GERD. The LES gets loosened, which allows acid to move up your food pipe. In fact, many surgical procedures that treat GERD focus on restoring the tonicity of LES by sewing a wire around it or tightening the opening.
GERD treatment options
The best approach to relieve the symptoms of GERD is by applying some lifestyle modifications that mainly focus on eating habits. Your doctor may also suggest one of the following pharmacological drugs to suppress the production of acid:
- Antacids
- H2 receptor blockers
- Proton pump inhibitors
The first class of drugs is usually appropriate for mild cases of GERD. When the treatment is not effective, the prescription of a strong H2 receptor blocker or a proton pump inhibitor becomes necessary.
If all treatments fail to improve the patient’s symptoms, the doctor may suggest seeing a general surgeon to discuss the potential procedures to cure GERD. Note that opting for a surgical solution is only on the table because of the potential complications of GERD.
Potential complications of GERD
The vast majority of people do not experience any serious complications of GERD. However, some rare cases can lead to life-threatening problems, including:
- Esophagitis – the inflammation of the food pipe
- Esophageal stricture – the narrowing of the esophagus due to tissue scarring after inflammation
- Barrett’s esophagus – changes in the cellular structure of the esophagus
- Esophageal cancer – only a small number of patients develop this condition. It almost always follows Barrett’s esophagus
- Asthma, chronic cough, or other breathing problems, which occur when the acid leaks into your lungs
- Tooth enamel erosion and gum disease
Preventing the symptoms of GERD by following your doctor’s instructions and taking your medications is the best way to reduce the risk of these complications.
Diet for GERD
Many people experience symptoms of GERD after eating certain foods, which are collectively known as trigger foods. These may include:
- High-fat foods
- Tomato
- Onion
- Garlic
- Mint
- Chocolate
- Spicy foods
- Citrus fruit
- Pineapple
- Alcohol
- Soda
- Coffee
- Tea
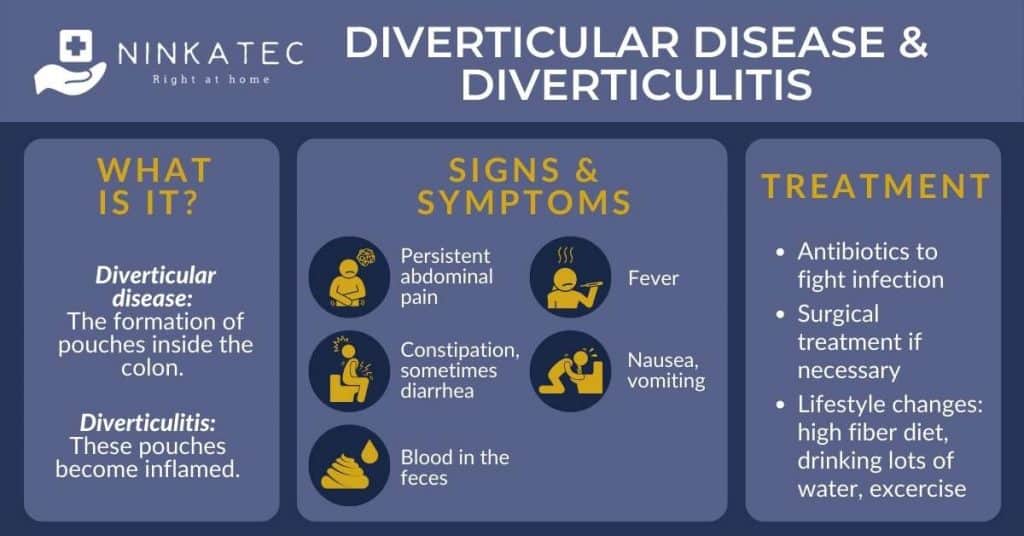
4. Diverticular Disease and Diverticulitis
Diverticular disease and diverticulitis are related gastrointestinal diseases that occur in the colon (i.e., large intestine). Diverticula refers to small pockets that can bulge out in the lining of the intestine, especially when you get older – a common issue in Singapore.
Diverticula does not develop any symptoms in most people. We might be unaware until after undergoing a CT scan or a colonoscopy for a different reason. Doctors refer to the presence of diverticula without symptoms as diverticulosis. If you develop symptoms, the condition gets another name – diverticular disease.
When the diverticula becomes inflamed, we call it diverticulitis – which means inflammation of diverticula in the medical terminology. Researchers found that people are more likely to develop diverticular disease and diverticulitis if they do not consume enough fiber in their daily diet.
Symptoms of diverticular disease and diverticulitis
If you develop diverticulitis, expect the following signs and symptoms:
- Severe, persistent pain
- Fever
- Diarrhea or constipation
- Blood in the feces
Treatment for diverticular disease and diverticulitis
Contact your doctor as soon as you notice symptoms of diverticular disease or diverticulitis, and especially when you notice any new symptoms (i.e., severe pain, rectal bleeding) accompanying those of diverticulitis.
Treatment of diverticulitis usually involves dietary changes to include more fiber. If there is inflammation, the doctor may prescribe antibiotics to treat the inflammation, in addition to diet changes. If inflammation does not improve with antibiotics or if the abscess is too large, diverticulitis may require surgical intervention.
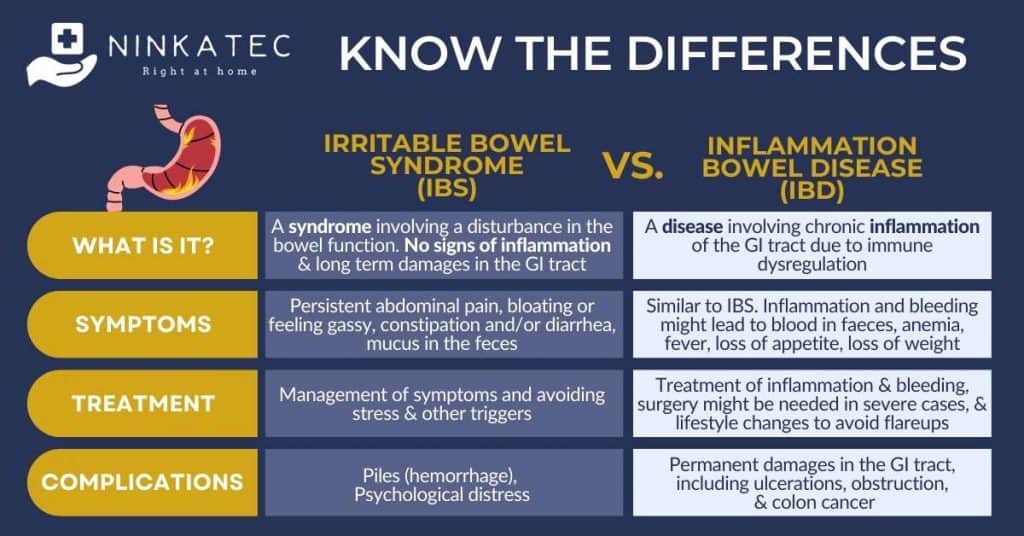
5. Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome, or IBS, is a syndrome, which means it is a group of symptoms rather than a disease. Despite having regular symptoms, patients with IBS do not show signs of inflammation or damages in the GI tract in the long term.
Causes of IBS
While the exact causes of IBS are not fully understood, the general cause is believed to be a disturbance in the bowel function. It is observed that IBS patients experience flareups when being under stress, after having a big meal or certain foods.
Symptoms of IBS
IBS symptoms include persistent abdominal pain, bloating or feeling gassy, constipation and/or diarrhea, mucus in the feces, and sometimes the urge to pass motion without being able to do so. Diagnosis of IBS includes elimination of other possible causes.
Treatment of IBS
IBS treatment focuses on the relief of discomfort and management of the symptoms that the individual patient experiences. Although there is no long term damages in the digestive tract, people IBS may encounter complications such as piles (hemorrhage) due to frequent constipation and/or diarrhoe, and psychological distress due to constant discomfort. Thus, treatment also aims to prevent and manage such complications early. Lifestyle changes to avoid stress and other triggers are also very helpful to manage IBS.
6. Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease, or IBD, can easily be mistaken with IBS by the general public, due to the similar names. In fact, they are 2 distinct conditions with different symptoms, causes and treatment.
IBD is a disease involving chronic inflammation of the gastrointestinal tract due to immune dysregulation. This chronic inflammation defines an important difference between IBD and IBS. Examination of the GI tract of a person with IBD often shows inflammation, ulceration, redness, or bleeding. Inflammation and bleeding cause distinct IBD symptoms that are not present in the case of IBS, including blood in feces, loss of weight and joint pain. The damages in the bowel caused by IBD can lead to much more serious complications compared to IBS, including precancerous change and even cancer of the colon.
There are 2 types of IBD, determined by the affected portion of the GI tract, as well as the underlying pathophysiology
- Crohn’s disease: any part of the GI tract can be affected
- Ulcerative colitis (UC): only the colon is affected
Unfortunately, there is no curative treatment for either disease, which leaves healthy lifestyle habits as the only possible way to temper down inflammation and decrease its toll on the digestive tract.
Symptoms of IBD
IBD often manifests with frequent and/or urgent urge to pass motion, abdominal pain or cramp, diarrhea and/or constipation which are similar to IBS. However, due to inflammation and bleeding, individuals with IBD may also experience blood in stool, anemia, fever, loss of appetite, loss of weight which are not typical in IBS cases.
What causes IBD?
As with most autoimmune diseases, the exact cause of IBS is unknown. However, researchers have successfully identified genetics and immune dysregulation as primary culprits. Here’s how it works:
- Genetics
You are more likely to develop IBD if you have a family member with this condition, which implies the potential involvement of a genetic component in the equation. Unfortunately, scientists were not able to pinpoint any gene or specific protein that causes IBD.
- Immune dysregulation
Generally speaking, the immune system launches an inflammatory reaction against pathogens in the gastrointestinal tract that try to invade your body. In healthy individuals, this reaction disappears shortly after the threat has been eliminated. However, patients with IBD live in a constant state of inflammation without any sign of foreign pathogen or active inflammation, which leads to the destruction of the patient’s own cells.
Note that a common trigger for IBD is a viral infection that occurs in the digestive tract, but inflammation does not stop after healing from the infection. This entire process is referred to as autoimmunity, which translates to the body’s attacking itself.
How does nutrition influence IBD?
While there is no specific diet that works perfectly for IBD, some food choices are effective in reducing inflammation and improving the clinical presentation of patients. For instance, loading up with probiotics and prebiotics was shown to be extremely beneficial for IBD patients in a 2020 study. Moreover, the elimination diet is also gaining some traction in this field since it allows patients to avoid any food that might potentially trigger inflammation in their gastrointestinal tract.
With that said, you will need the help of a professional to design a tailored dietary plan that matches the severity of your condition, the frequency of flare ups, and the type of medications you are taking.
7. Gastroscopy and Colonoscopy - Effective Ways to Look Inside the GI Tract and Diagnose GI Diseases
Screening for gastrointestinal diseases with the help of an endoscope is extremely effective at detecting severe conditions early. Depending on the location of your symptoms, your doctor may opt for:
- Gastroscopy or upper gastrointestinal endoscopy – covers the esophagus, stomach, and the first part of the small intestines
- Colonoscopy or lower gastrointestinal endoscopy – covers the anus, rectum, and colon
These procedures allow the doctors to take a look inside the digestive tract, examining signs of inflammation, bleeding and polyps. Certain types of endoscopy allow doctors to perform additional procedures such as removal of polyps on the flight. Samples from the polyps (biopsies) are then sent for lab analysis to confirm if the polyps are benign or cancerous.
Gastroscopy can be performed with numbing the throat while colonoscopy is often conducted under sedation. Preparation for the 2 procedures also differs. Patients only need to fast for 8-12 hours before a gastroscopy but need to cleanse the bowel for colonoscopy. Bowel preparation for colonoscopy involves low or no fiber diet 2-3 days before the procedure and taking bowel cleansing solutions 12 hours before.
Apart from helping doctors diagnose GI diseases, colonoscopy is one of the most effective tools to screen and detect colorectal cancer early. It is currently recommended for everyone above the age of 50 in Singapore. Find out more about colorectal cancer, risk factors and screening recommendations in our dedicated article here.
8. Manage Gastrointestinal Conditions at Home with Ninkatec
While some of these common gastrointestinal diseases need to be managed actively at home with diet and lifestyle changes, other conditions may require consultation with a doctor on urgent or regular basis. Ninkatec is one of Singapore’s leading home care service providers. Our technology allows us to provide personalised care and deploy prompt response to patient’s condition developments, all in the comfort of your own home. Do not hesitate to check in with Ninkatec’s friendly care team if your loved one is experiencing gastrointestinal symptoms that might require doctor consultation.